You might think salt makes you bloated. It's actually something else. We hear all the…
More About Cholesterol Pills
The Nitty Gritty
For those of you who want to know more than I posted here this is a slightly more technical section.
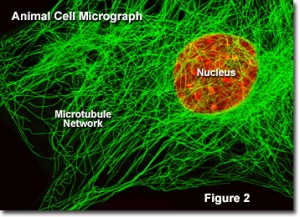
The image on the top is a view of the skeleton of your cells. The whispy green fibers are called the cell’s cytoskeleton. This is what makes your cells durable. Without a cytoskeleton, your cells would disintigrate on contact, your tissues would have the consistency of a thin soup, and life as we know it would not exist.
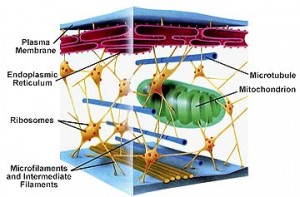
The next image shows how your cell compartments, called organelles, are held in place by microfilaments and intermediate filaments which are part of the cell’s cytoskeleton.
This article is continued below...(scroll down)
Cool, huh? I think so.
But it’s not so cool that the most popular, most prescribed drugs in the country, the cholesterol lowering pills called statin (Lipitor, Zetia, Vytorin, Zocor are popular examples) can destroy the exquisitely intricate architecture of your cytoskeleton and prevent a whole host of cells in your body from working normally, from liver cells, to immune system cells, to muscle cells (including the muscle that is your heart), to brain and nerve cells. Here’s how they do it.
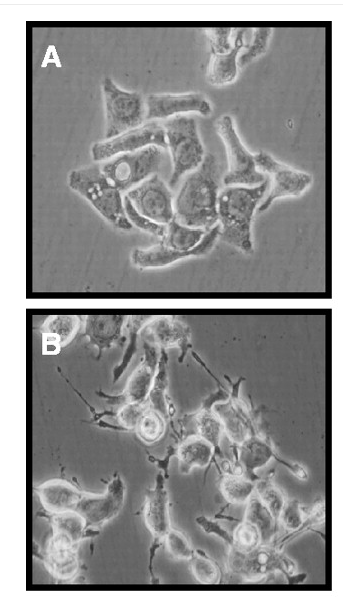
Statins block important metabolic pathways called Mevalonate pathways. One of the most important Mevalonate pathways forms the cytoskeleton. The cytoskeleton supports the shape of your cells, and controls all substructural movements, including the division of the cell during replication, the distribution of nutrients and energy throughout the cell’s compartments, and synthesis of proteins and hormones. Many people on statins suffer from unrecognized effects of blocked Mevalonate pathways.
The side effects of these blocked pathways and the resulting cytoskeletal malfunctions are diverse, and include cancers, memory loss, nerve pains, and muscle weakness. Accordingly, statins have been shown to cause breast cancer, skin cancers, confusion, concentration problems, depression, kidney damage, liver damage, and high sugar levels—thus explaining the fact that being on a statin increases your risk of diabetes by 50%. Statins are so powerfully and reliably able to destroy the cytoskeleton, they are used as research tools to understand what role the cytoskeleton plays in metabolism; researchers infuse cells with small doses of statins to impair, for instance, the ability of a cell to manufacture nitric oxide signals. Once the associated cytoskeletal structure disintegrates, researchers stand back and watch what happens when the cell can’t make nitric oxide. The more researchers work on this issue, the more they discover that damage to the Mevalonate pathways and the cytoskeleton can cause all kinds of chronic diseases and cellular malfunction.
Fortunately, some people on statins are able to avoid cytoskeletal damage because their metabolic pathways can take alternate routes to manufacturing cytoskeletal components. However, during stress, infection, or with diet changes, this ability may be lost.
Many people are not able to fully bypass the metabolic blockages caused by statin drugs. These people often experience minor side effects, including fatigue, body aches, and subtle memory problems (“senior moments”). Unfortuntately, these are also the kind of symptoms most people might attribute to aging, and people continue their drugs, as more damage occurs.
Muscle cell damage can progress to atrophy and weakness, and because the heart muscle cells are affected to, can even lead to heart failure. Ironically, this means that statins, which many people take because they want to protect their heart, are actually quite likely to increase their risk of dying from heart disease. (Heart failure deaths have been on the rise since the introduction of statin drugs.)
Nerve cell damage can cause burning pains, especially at night, as well as major depression, balance and coordination problems, and even total amnesia. Some of these symptoms resolve with cessation of the medication, but not all. Because the current guidelines now state that all diabetics with LDL over 100 should be on statins, it is especially important for diabetics to be aware that statins increase their insulin requirements and can make it harder to control blood glucose levels.
Who should take statins?
I recommend statins to all men who smoke and who have had a heart attack already. Studies clearly show benefit in this small subpopulation. In male smokers who have had a heart attack and are not taking aspirin, statin drugs reduce the chance of dying in the next five years by six percent.
Are you saying that all the good things I hear about statins are false?
TV advertisements and medical education classes are carefully worded to be as true as possible. So while not always false, they are very misleading. You will not see this language, for instance, in a drug company advertisement for cholesterol pills: “cholesterol causes heart attacks.” Why not? Because cholesterol does not cause heart attacks.
As another example, lets analyze two misleading claims in the following statement: Statins reduce the risk of heart attack by up to 30% in some high risk groups.
The first misleading claim is the risk reduction of 30%. Here’s what the studies do to come to this conclusion. They start with, say, 100 high risk people. Lets make them male smokers. All of them have a family history of heart attacks. It doesn’t matter what their cholesterol levels is. They put all of them on statins and they’ll keep taking the drug for five years. Meanwhile, they’ve gotten together another group of 100 high risk people, again male smokers with a family history of heart disease and comparable cholesterol levels. This group doesn’t get the statins, its called the control group. Over the course of five years, two men in the statin group and three men in the control group have heart attacks. Two is (about) 30% less than three, so although only one man in the group of 100 men on the drug was saved from a heart attack, because they use the terminology “risk reduction” they aren’t exactly making a false claim. It would be more accurate to say something like this: One high risk smoking male in a hundred will be saved from a heart attack by taking statins, as long as he takes it for five years.
Notice I didn’t say “one in a hundred will be saved from death.” This brings me to the second point of misdirection. The vast majority of statin drug trials fail to show any benefit on mortality. In other words, although they do prevent (some) people from dying from heart attacks, people die slightly more often from side effects of the drug, so the overall survival effect is neutral.
Furthermore, the designers of the drug studies are careful to exclude people who are likely to die from the side effects of their drug. They do not allow people with a history of cancer, heart disease, uncontrolled diabetes, or certain other medical problems to participate in statin drug trials. If these people were not excluded, many scientists believe that by the end of statin drug trials, more people would be dead from side effects of the drug than were saved from having heart attacks.
Who should NOT take statins?
Women, children, and men over 65. Studies have not shown that statins offer any mortality benefit to these groups of people. However, when statin drug experts are interviewed and this fact is pointed out to them, these professionals generally respond by reminding us that there is no study proving that statins are not beneficial. In other words, the burden of proof is now on patients to provide the doctors with evidence that they should not take the drug. Since its impossible to prove a negative, the experts are asking us to ignore the science we do have, and instead dive into the murky realm of their own (biased) personal belief systems.
But my “bad” cholesterol has gotten better since I started taking statins, doesn’t this mean the drug is helping me?
High total cholesterol is not a risk factor for heart disease. High LDL cholesterol (LDL is called “bad” cholesterol) is only weakly correlated with heart disease. So lowering everyone’s LDL cholesterol with pills will not help most of the population. After thousands of studies and millions of dollars, the evidence still shows only those men who smoke and who are not on aspirin actually benefit from the pills. And their benefit does not correlate with cholesterol lowering.
In recent years, mounting evidence has shown that cholesterol is not the cause of arterial damage that leads to heart attacks. Oxidized fats, nutrient deficiencies and high blood sugar levels all play a role. Everyone agrees that normal, non-oxidized cholesterol plays no role, but the popular press and even medical journals downplay this fact. Furthermore, most lipid scientists acknowledge that LDL cholesterol plays no role; only oxidized LDL particles are a problem. How are LDL particles oxidized? That’s a good question, and I answer it in Deep Nutrition, Chapter 7, entitled Good Fats and Bad..
Why does my doctor tell me to take statins?
You probably have heard about drug companies influencing doctors by buying us free lunches or sending us on expensive vacations. I can tell you this influence is relatively minor; I wouldn’t change my prescribing habits or recommend drugs that I thought were dangerous just because I once had a nice meal paid for by the company that sells them.
What you probably haven’t heard very much about is the fact that drug companies have enormous influence over the medical education system. In other words, much of what your doctor learns (and is repeatedly tested on to keep his or her license) was approved by drug companies.
How can big pharma have so much influence over science? It’s simple economics.
Most doctors read medical journals. In order for medical journals to pay their bills, they have to advertise. This means they depend on drug companies for survival. If an editor publishes any article that portrays a drug as dangerous, he risks loosing the magazine’s source of income, and that means he risks loosing his job. (For more, see On The Take by former New England Journal of Medicine Editor, Jerome Kasserier.)
If statins are so dangerous, why aren’t we seeing people drop dead from them?
I think we are. You’ve probably heard about the Institute of Medicine’s report on doctor/hospital induced injuries, citing that nearly half a million deaths per year are complications of medical care. Many of these people died while admitted to the hospital for heart failure, and statins cause heart failure. Others in the study had cancer and died of infectious complications of their chemotherapy. You probably haven’t heard about this, but many studies have shown an association between low cholesterol and death from cancer and infectious disease, so there is reason to be concerned that on statin medications doctors are reducing their patient’s cholesterol to dangerously low values. Because statins and cholesterol that is too low both can cause so many different metabolic problems, this actually makes it harder for statisticians to notice a blip in any one disease induced by statin medications. And since doctors don’t hear about the potential harms statins may cause, they have no reason to suspect statin drugs may be the culprit when new medical problems arise, or old ones worsen.
I have had only three of my patients develop and ultimately die of cancer while under my care, all had been on statins before I understood their risks. I have had several of my patients develop heart problems (heart failure and arrythmias) while on statins after having a heart attack. The scary thing is that cardiologists don’t believe there is any risk to taking these drugs, mostly because they don’t try to understand how they work.
It’s not just cardiologists who are prescribing powerful drugs that they don’t understand. Neurologists also start patients on statins because they believe that statins reduce the risk of strokes. Unfortunately, while there may be some truth to that, all such studies have been designed and paid for by drug companies, and I don’t have much trust in their findings given this scenario. Meanwhile, most neurologists have not heard, or refuse to believe, that statins damage nerve cells and therefore deny that extended use may wind up causing more neurologic disease than they can possibly prevent.
If statins won’t help reduce my risk of having a heart attack, what will?
The most important thing you can do is make sure you eat a balanced diet of fresh foods. Fresh is the key term, as nutrients are rapidly lost with the passage of time, with cooking, even with washing and slicing. See the rest of my web site for more details on getting the nutrients you need.
Men can reduce their risk of heart attack by 25% by taking 81 mg of aspirin every day. Fish oils also help, but getting a high-quality fish oil is key. I’ll be posting on supplements soon.
“We still don’t know how statins work, but I haven’t stopped prescribing them.”
–Dr. Douglas Losordo, chief of cardiovascular research at St. Elizabeth’s Medical Center in Boston.
Flippant remarks like this are common among statin drug proponents. But if statin experts are recommending that nearly 40% of the population take these medications, shouldn’t they be just a little bit more curious about what they do?
Confusion Among The Ranks
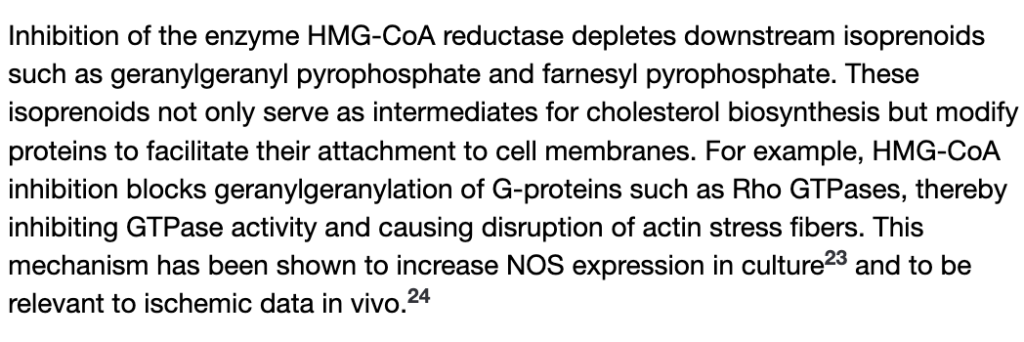
The history of our faith in statins begins with one basic fact, statin drugs block an enzyme (called HMGCoA reductase) which is one of many enzymes along the metabolic path to manufacturing cholesterol. Statins are very effective at lowering cholesterol because of this blockage. But this impressive ability to lower cholesterol doesn’t translate to saving lives. Indeed, experts seem confused as to whether the modest beneficial effects of statins are from the cholesterol lowering effects, or from the effect of reducing some other chemical or groups of chemicals:
Dr. Paul Ridker at the Brigham and Women’s Hospital reported in The New England Journal of Medicine that statins reduced heart disease risk even in patients with otherwise healthy cholesterol levels, provided their CRP levels were above normal. “What was extraordinary,” says Ridker, “was that the drug was just as effective in saving lives in the absence of high cholesterol, if the CRP [level] was high. Not only are these drugs ‘anti-inflammatory,’ as well as lipid lowering, but now there’s actually clinical evidence to show that perhaps the way we prescribe these drugs needs to be rethought, because people with low cholesterol can still benefit from these drugs if they have an inflammatory response.”
So the drug doesn’t work by lowering cholesterol, it works on people with high CRP? Other studies say no. But even if it does work on people with high CRP rather than high cholesterol, it would be nice to sort this out in order to be sure to give the drug to the right people at the right time, rather than the shotgun approach we take today. Unfortunately, there is money being made selling these drugs to as many people as possible, whether or not they’ll do more harm than good. And that golden glow over the eyes of academicians involved in drug studies is effectively obscuring intelligent insight into who should take the drugs, and when they should be taken.
Raising “Good” Cholesterol (HDL) With Drugs Might Kill You
From The New York Times, Dec 4, 2006:
Pfizer’s most promising experimental drug [torcetrapib], intended to treat heart disease, actually caused an increase in deaths and heart problems. Eighty-two people had died so far in a clinical trial, versus 51 people in the same trial who had not taken it….Shortly after 9 p.m. Saturday, Pfizer announced that it had pulled the plug on the medicine entirely, turning the company’s nearly $1 billion investment in it into a total loss.
The lipid cycle explains why these drugs don’t work
The lipid cycle is my term for describing the flow of fats throughout our bloodstream. (I added the term to Wikipedia.)
The lipid cycle was perfected by evolution millions of years ago to solve the problem of distributing fatty materials throughout a watery bloodstream. The solution was to wrap ingested fat in protein, thus making lipoproteins. When doctors talk about HDL and LDL, or so-called “good” and “bad” cholesterol, they’re talking about lipoproteins.
In those, good ‘ol days when jellyfish ruled the Earth, there was no such thing as man-made toxic fats like trans fats. Burnt and oxidized fats were also rare because cooking was not invented. Cholesterol is just one of many types of fatty nutrients that must circulate within lipoproteins, others include essential fatty acids like omega 3, fat soluble vitamins A, D, E, and K, and choline. All nutrients must circulate throughout all organs of the body to ensure adequate and equitable distribution to tissues in need.
The lipid delivery system was simply not designed to deal with toxic fats we have in our diets today. When fats are oxidized, the lipid cycle doesn’t function properly, and this may result in increased LDL and/or triglyceride levels and, ultimately, heart attacks and strokes. Furthermore, since the function of lipoproteins is nutrient delivery, if your lipoproteins are damaged by toxic fats your tissues may not get the vitamins they need – and you get sick.
The lipid cycle can be partially disrupted by various drugs. Statins make it hard for the liver to synthesize new cholesterol for release into phase two of the lipid cycle by inhibiting an enzyme called HMGCoA reductase. This is how statins make LDL levels fall. When the liver cannot make its own cholesterol, HDL levels may rise. HDL has been dubbed the “good” cholesterol because high levels are associated with longer life. (Probably because high HDL indicates a well-balanced lipid cycle.) When the HDL rises due to statin ingestion, it is not a sign of a healthy, balanced lipid cycle, it is a side effect of a disrupted lipid cycle. If LDL has been reduced, the step in the cycle whereby HDL transfers its apoproteins to LDL occurs less frequently and the apoproteins remain stuck on HDL, making the levels of HDL rise. Pfizer’s latest debacle interfered with the lipid cycle more directly than statins do, and with deadly results.
Another Way Statins May Help Some People
The evidence clearly shows that statins reduce incidence of heart attacks in some groups of people while they increase the incidence of other fatal illnesses in many. The one group of people who truly benefit from statins are male smokers who have already had a heart attack. This section discusses how statins helps them die 6% less often (over 5 years) then they would without statins.
I’ve already suggested statins have a mild anti-inflammatory effect that may prevent blood clots, here. But a relatively recent study suggests an additional beneficial effect may be in the prevention of excessive or abnormal blood vessel constriction.
Blood vessel constriction can lead to heart attacks and even fibrillation and death. One trigger for blood vessel constriction is release of a neurotransmitter called acetocholine from nerve endings. Excess acetocholine release occurs during exercise, emotional stress, or illness.
In a recent study, (Heart. 2006 Nov;92(11):1603-9. Epub 2006 May 18.
Short-term statin treatment improves endothelial function and neurohormonal imbalance in normocholesterolaemic patients with non-ischaemic heart failure) statin infusion was shown to blunt excess acetocholine release and prevent dangerous blood vessel constriction.
Nicotine is known to cause blood vessel constriction, which may be one factor in why smokers have more heart attacks than nonsmokers. So smokers who have had a heart attack will suffer less from the effects of their continued smoking while on statins. Unfortunately, studies have only shown this benefit over a five year period. The trouble is, the longer a person smokes and the longer a person takes statins, the more likely they are to develop cancer. So for you male smokers who have already had a heart attack, talking statins may end up killing you more often after 5 years than not taking statins, we still don’t know.
Please note: Please do not share personal medical information in a comment on our posts. It will be deleted due to HIPAA regulations.
This Post Has 2 Comments
Note: Please do not share personal information with a medical question in our comment section. Comments containing this content will be deleted due to HIPAA regulations.

















Well written article. Would you Dr Crate be willing to be interviewed for a programme we are going to make soon for the BBC in the UK?
Mahalo Dr. Cate for your well-written, detailed explanation of how our cells and cholesterol tie into each other to keep us alive and healthy and how statins can disrupt this delicate system. I just listened to a podcast from the Therapuetics Initiative at University of British Colombia (http://ti.ubc.ca/en/node/205) and learned that the benefits derived from taking statins was not that impressive when talking in absolute terms. For primary prevention the absolute risk reduction for major coronary events was 1% to 1/5%, for diabetics it was 2% and for secondary prevention it was 4% all with a catch that those benefits can only be derived if one takes the statin for at least 5 years. Can you imagine the damage that can result from statin side effects during that time? Very scary. Mahalo again for having the courage to speak out on this issue.