You might think salt makes you bloated. It's actually something else. We hear all the…
Statin Side Effects Slowing You Down? Why your doctor may not be able to help.
A new plan unveiled this week by the Department of Health and Human Services will make it more difficult for a patient to have an open and frank discussion with his doctor about the potential side effects of statin medications.

It’s no secret that statins, taken to reduce your risk of heart attack and stroke, can have serious side effects (that include developing diabetes); simply read the package insert. It’s not unusual that, when reviewing a new patient’s previous charts, I see they have experienced symptoms potentially attributable to their statin prescription(s). Sometimes the nurses’ notes even document that the patient expressed concern that their symptoms might be the side effects of their statin medication(s). Often, however, the record shows that their doctor’s response was to simply scribble out another prescription to treat the new symptoms.
When you talk “privately” with your doctor, is someone else in the room with you?
Few people know that when a patient has a private talk in the exam room with his personal health care provider, he is often not—as much as he might like to believe—having a one-on-one conversation. Any time you are on a medication you suspect may be hurting you, and you go through the “ask your doctor if you are experiencing” routine, the answers you get may depend on what your insurance company wants your doctor to say.
This article is continued below...(scroll down)
It works like this. Right now, a small portion of the money you pay for health insurance is allocated to your doctor through a system of evaluations called “pay-for-performance.” When the health insurance company agrees with what your doctor is doing, the doctor is paid better. When the health insurance company disagrees, your doctor is financially penalized.
Pay for Performance: How corporations get doctors to do what’s good for you business
Insurance companies argue that pay-for-performance helps ensure that physicians make recommendations in the best interest of patients, and that these financial incentives (or penalties, depending on your point of view) help elevate “standard of care.” Whether or not one agrees with this, it’s clear that a more accurate term for the policy would be “pay for compliance,” and that such policies are likely to influence what your doctor is telling you. That is, after all, why these incentive policies were created—to influence physician care.
But there is at least one potentially serious side effect from insurance companies prescribing physicians’ recommendations: By incentivizing your doctor to make a recommendation he or she might not have made without the threat of financial penalty (or the promise of financial reward), insurance companies have placed themselves squarely between you and your doctor, intruding on this most sacred of relationships. With this new Department of Health initiative, whatever distractions that financial reward creates in your doctor’s mind as he listens to what you are saying and makes decisions about your future, that influence is about to grow much louder. The insurance companies will no longer merely be whispering in your doctor’s ear. They’ll now be “guiding” his recommendations through a bullhorn.
And this is why it has become especially important to ask him or her how likely it is that the drugs you take will actually help you, and to demand a lucid and detailed answer.
It’s also a good idea to get a second opinion, perhaps from a book
If you are familiar with my books, you know I’ve combed through a staggering amount of research and have yet to uncover a shred of compelling evidence tying LDL cholesterol to heart attacks. And if you’ve read Dr. Atkins, Gary Taubes, Mark Sisson, Robb Wolf and other nutrition luminaries, you know they have drawn the same conclusion: No solid evidence indicts cholesterol as the cause of heart disease. A new book by a cardiologist, out just last month, is joining the discussion, and it’s already a best-seller (Wheat Belly by Dr. William Davis). The gears of the anti-cholesterol machinery are slowly seizing up.
If you’ve read my books, you also already know that the stuff in our bloodstream that causes heart attacks is not happy normal cholesterol in happy normal LDL or HDL, but oxidized lipoprotein particles that became oxidized from a diet high in sugar and trans fat and lacking in nutrients. This assertion is not controversial; all lipid specialists agree. Currently though, I’m sorry to say, we have no test to measure just how many oxidized lipoprotein particles you have in your bloodstream. So we fudge it; we call LDL “bad cholesterol.” And for the giants of the pharmaceutical industry, that way of thinking about cholesterol works just fine: “Got bad cholesterol? No problem. We’ve a drug for that. And we pay our doctors in such a way that they forget that, like any other drug, statins have side effects, too.”
So are statin drugs “right for you,” or not?
A good way to determine how likely a drug is going to help is through a statistic called the “number needed to treat,” or NNT for short. If the NNT is low, say 5 or 10, that means that only 5 or 10 people just like you have to take the drug to prevent the occurrence of, say, a single heart attack.
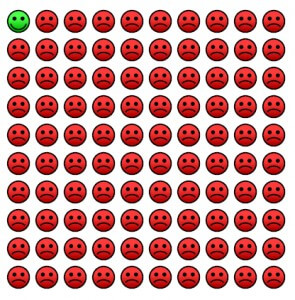
Statistics show that the NNT for statins is much higher than you might think, particularly given all the hype about how important they are for your health. The lowest reported NNT is 30, in male smokers who have already had one heart attack. For the average person with no history of heart attack, who doesn’t smoke, and who doesn’t have diabetes, it’s over 100.
Here’s an article that describes the problem:
“Another serious problem with the way the results are presented [to your doctor] is that the reader is often not told the number needed to treat (NNT) for one patient to benefit. The NNTs range from around 30 in the 4S and LIPID trials to over 100 in the primary prevention trials. But this is not the information that patients are likely to be given; instead, they will be told that they will reduce their risk of death by about 30%. Presenting information to patients in the form of relative risk will much increase their receptiveness to taking the drug.”
There’s another important number you want your doctor to be able to tell you: the number needed to harm. Unfortunately, because not too many drug companies are fond of funding research like this, there are precious few statistics published about the number of patients harmed by statins. One example I did find is for renal failure in women: the number needed to harm is only 434. That’s one side effect. Another is the development of diabetes: that’s 498. Cancer may need to be included as a side effect because in one study that was stopped early, The Effect of Pravistatin on Coronary Events after MI in Patients with Average Cholesterol Levels NEJM 355:1001-1009, 1996, 14 women on a statin developed a recurrence of their breast cancer compared to only 1 on the placebo. (The cancer association was much stronger than the effect of premarin on breast cancer, and that statistic led to a storm of media coverage.)
Statins can also cause severe liver dysfunction. Number needed to harm: 136. And cataracts: NNH=32!! You get the point.
A recent article in American Family Physician puts my gripe about misinformation rather well:
“With a NNT above 75, a number needed to harm would be helpful in determining if we should prescribe these medications to our patients.
It would be interesting to see if a patient’s decision whether or not to take the drug was influenced by using one of the following statements: ‘This drug will decrease your chance of dying by 12 percent.’ Or, ‘Out of the 167 patients that take this pill for the next four years, one patient will not die who would have if he or she had not taken the drug, but 166 will take the medicine and get no benefit, and may be harmed.’
There is a big difference between relative and absolute risk reductions. Conveying the NNT to our colleagues and patients provides a more accurate assessment of the effectiveness of a drug, and might help physicians and patients make more informed decisions.”
Statins can help some people, some of the time
The oxidized-lipoprotein-particle reality I mentioned above is the reason why the average person with high cholesterol is actually a teensy bit more likely to have a heart attack than the average person without high cholesterol. They are more likely because they have more particles vulnerable to oxidation, but only that teensy bit more likely, and that is only true if one is on the average (pro-inflammatory) diet. Therefore statin drugs are only a teensy bit likely to help the average person (who has not already had a heart attack, smokes, or has uncontrolled diabetes) on the average diet.
I have to say this next bit by way of disclaimer, but it’s also true: if I were your doctor, I would only stop these medications after sitting down with you and asking enough questions to get a realistic assessment of your risk of heart attack. As an essential part of your care, I would provide you with nutrition advice that would make you virtually heart attack proof by protecting your LDL (and other lipoproteins) from harmful oxidation events.
Unfortunately, though the diet I advise may make you virtually heart attack proof, if it fails to get your LDL number down to where your insurance company thinks it needs to be, I will be financially penalized.
On a positive note, if I may quote Nan from TrueBlood, my lastest favorite show, “There are factions inside the regime who have never been completely on board with the current agenda.” What I’m saying is, there are still doctors who will, believe it or not, refuse to play the pay-for-performance game—and take a financial hit for doing so. And there are hospitals and medical centers who still encourage doctors to keep their patients fully informed. Not sort of informed. Or “informed” in quotes—informed only so far as your insurance company wants you to be—but informed. Not many, but their numbers are growing daily.
That’s right. The sanctity of the patient-doctor relationship is not without its defenders. I’m talking about good doctors, good hospitals and knowledgable, conscientious patients who want to know what their trusted family physician really thinks.
In other words, people like you.
Check out these links for a good doctor in your area:
http://primaldocs.com/
http://lowcarbdoctors.blogspot.com/
http://paleophysiciansnetwork.com/
And this link is to a list of articles by the author of Wheat Belly, who is that rarest of animals a cardiologist who has a balanced view of the utility of statins: http://www.trackyourplaque.com/blog/category/statin-drugs
Please note: Please do not share personal medical information in a comment on our posts. It will be deleted due to HIPAA regulations.
This Post Has 8 Comments
Comments are closed.
Note: Please do not share personal information with a medical question in our comment section. Comments containing this content will be deleted due to HIPAA regulations.

















Thanks Dr. Cate. Very informative blog! In my case though, I’ve had type one diabetes for 44 years and had by=pass surgery 3 years ago. How do I determine if I really need to be on statins or not? I have been on a low carb/complex carb diet with low animal protein for a while now. This is a very confusing topic.
Thanks,
Gary
Gary you are one of the millions of Americans learning about this topsy turvy world of fats and suddenly finding themselves caught between their cardiologist and a hard place. You are unlikely to find a cardiologist who is willing to consider stopping a statin, now that you’ve had surgery. If you never actually had a heart attack and did not have heart failure, you may be able to argue that the evidence for the bypass benefitting you was limited and now you are concerned about further deepening the damage done by the continuation of a statin.
In chapter 8 of Deep Nutrition I describe the great leap it took for me to open my eyes to the reality of what really causes heart disease, and therefore what should be done about it. That chapter should greatly help your understanding of what to do.
Hi Al! Nice to hear from you!
Any of the low-carb doctors : http://lowcarbdoctors.blogspot.com/
or paleo doctors http://robbwolf.com/2011/02/08/paleo-physician-network-is-live/
Keep reading, and stay sharp!
Dr. Cate,
Is there any Dr. in Manchster who thinks as You do? If so, name please. You are in total agreement with the big boys i.e.Jonathan Wright, Bruce West, Robert Rowen, Frank Schallenberger etc. who are all on the west coast. Now we add Cate Shanahan to the list. Please don’t change and succumb to big pharma. Thanks again for treating us while you were here. Regards,
Al & Polly!
Hello Dr Cate! I bought your book two weeks ago after listening to your Underground Wellness podcast. My boyfriend and I have been eating healthier over the past months, getting really great improvements in our moods and energy levels from getting rid of sugar and wheat. We were considering transitioning to Paleo but thought we would really struggle to also stop eating dairy, legumes and all grains. After listening to you on the podcast I bought Deep Nutrition on Kindle and devoured it in three days. It made me so excited to start the diet changes- not Paleo but traditional!
We cooked our first organic grass-fed lamb leg roast last weekend- five hours in the oven! Tasted like heaven and we had leftovers for the next two nights as well. Am kicking myself I didn’t stop my boyfriend from throwing out the bone when he went and did the washing up. We do have another leg in the freezer though and he now knows all bones are to be kept for broth. This weekend I’m going to do a whole organic roast chicken in our slowcooker, and make some broth with those bones. I have a problem with pain in my knee when I run and am hoping the glucosamines might improve things. I am working up to trying liver, I’m still slightly queasy on the idea but am gaining courage when I think about how good it will be for me. Just need the right recipe. This week the only grains I have eaten have been sprouted quinoa, I even made some essene bread with it (need a bit more time to experiment with it I think). I am eating lentils and beans, we found an organic grocer selling unpasteurised butter and are frying our morning eggs and bacon in it. I am eating whole milk yoghurt first thing in the morning. I am snacking on nuts and cottage cheese and lupini beans.
I am SO SATISFIED by the food I am eating!!!! This is so huge for me, as I am- well WAS that person who is ALWAYS HUNGRY even if I’ve just eaten. I’ve been reading through your blog here too and your May entry about how much carbohydrates we ‘need’ each day has made me feel safe to pretty much dump starchy carbs altogether- which have always made me feel fuzzy headed and hungry and BLOATED. I just didn’t see how I could be without them as I craved them and in fact it made me doubt whether I could maintain Paleo, because Paleo disallows legumes and I thought I couldn’t lose both. When I’m having a meat or bean meal with salads and veggies my stomach is staying pretty flat- I never thought I could have a contendedly full stomach without it puffing out!
I wanted to ask if you and your publisher would consider enabling Deep Nutrition for sharing on Kindle devices. I wish I had bought a hard copy of the book because I want my parents and sister to read it; I’m also really keen to have two members of my bookclub read it as they are trying to get pregnant and I know they (and their future babies) would benefit so much from the info in Deep Nutrition. They wouldn’t seek the book out on their own because the information is just too diametrically opposed to the mainstream ‘healthy eating’ propoganda they have been bombarded with. But I have piqued their interest because they could see how adamant I was and as I explained some of the science and logic of your book. I said I would see I could share it with them via their Kindles, but discovered it was not enabled. While it might seem that authors and publishers would lose out on potential sales by enabling lending, I wanted to suggest that for a book such as yours the lending program (which I understand allows lending to up to six people from one kindle book purchase) has fantastic potential spread your influence and message and reach people who wouldn’t ordinarily be inclined to pick it up on their own but would read it if it was loaned from a friend.
Thankyou so much for writing this book! Food Rules is next on my reading list, and I’m so excited to hear you are now writing the TRIM book, all my very best :o)
Emily
Josh
Me too. But I do know a few good men and women in the business, and I like to think our numbers will grow and our patients will flourish.
Awesome post.
To be honest, the direction modern medicine is going really scares me. It’s hard to say if we’ll actually see a paradigm shift in the near future, or if things will get worse before they’ll get better. On one hand it’s encouraging to see people like Robb Wolf and Mark Scisson make it somewhat mainstream, but “new plans” like this make things seem a bit more gloomy.
Josh
Hi Dr. Cate, Very informative post, Thanks! It made me think back to a post on Dr. Davis’s blog:
http://www.trackyourplaque.com/blog/2010/10/medical-education-in-the-days-of-big-pharma.html