If you’re trying to get healthier, you probably want to know where to focus your food efforts. Should you spend extra on organic to avoid glyphosate? Or avoid seed oils? Which change will actually protect your health the most? This post will help you understand that there is one clear answer according to science.
Who Teaches Doctors About Cholesterol-lowering Drugs?
Table of Contents
- The Incredible Shrinking LDL Cholesterol Target
- The Perils of Low Cholesterol
- Doctors Writing LDL Cholesterol Guidelines Need Money for Research
- Independent Physicians Call for Less Aggressive Cholesterol-Lowering Guidelines
- Well-funded Experts Slam Independent Reviewers
- Doctors Unaware or Unconcerned About Conflicts of Interest in Science
- Conflicted Journal Editors Don’t Print the Whole Truth
- What Can You Do?
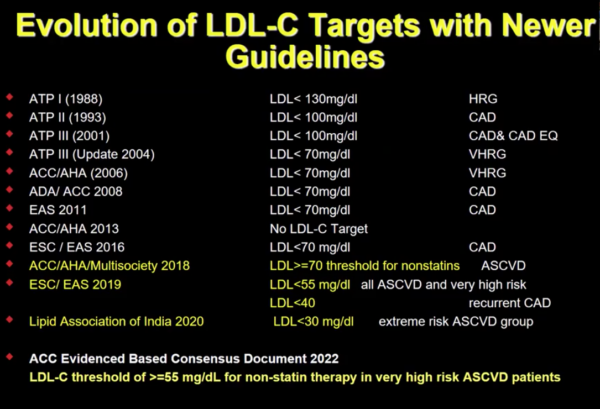
It might seem like the science linking cholesterol to heart attacks is solid. It might seem like doctors know for sure where your cholesterol numbers need to be. But did you know that the number considered low enough has had to shift downward multiple times? Cholesterol-lowering “targets” are lower today than ever before.
If you don’t already know, LDL cholesterol is a kind of particle that circulates in our blood. It acts like a delivery vehicle for specific nutrients, including cholesterol itself. Most doctors believe these LDL cholesterol particles can cause heart attacks, and call LDL the “bad” cholesterol.
Cardiologists often talk about cholesterol as if it were a toxin. But cholesterol is not a toxin. Cholesterol is a building block for hormones like testosterone and for our body’s cell membranes.
This article is continued below...(scroll down)
What’s more, our efforts to prevent heart attacks by cutting cholesterol haven’t worked as well as planned. For example, in 2009, a study showed that most people with heart attacks already have low cholesterol
So what did our guideline makers do? Instead of questioning our heart attack prevention strategy, they’ve moved the goalposts.
The Incredible Shrinking LDL Cholesterol Target
When I entered medical school, the acceptable LDL cholesterol level was 130. The number was 160 just two years earlier. The rules of the cholesterol game have changed not just once, but quite a few times. Isn’t that a little strange?
The slide below shows that the acceptable LDL level has been cut 6 times so far, and is heading for a 7th. I got this from a presentation for cardiologists at a 2023 conference in California.
The educator who created this slide has impeccable-seeming credentials. He is a fellow of multiple medical societies ostensibly devoted to the prevention of heart disease, the American College of Cardiologists, the American Heart Association, The National Lipid Association, and the American Society of Preventative Cardiology. And he is president or past president of a couple of these associations. Even more impressive, he’s also the director of the Heart Disease Prevention program at UC Irvine and Co-editor-in-chief of the American Journal of Preventative Cardiology.
In other words, doctors are very likely to believe him. When he says that we need to eradicate most LDL cholesterol from our bloodstream, his word carries a lot of influence. Doctors assume he’s saying it because evidence backs him up.
But as a doctor myself, I can tell you levels under 70 are exceptionally low. And under 30 is almost impossible unless you are severely malnourished–or taking multiple cholesterol-lowering drugs. Subjecting people to such extreme cholesterol-lowering therapy is essentially an experiment.
The Perils of Low Cholesterol
I’ve written about several problems linked to low cholesterol. There is a link between low cholesterol, dementia and neurodegeneration. This article discusses the early findings that people with lower cholesterol are more likely to die from COVID (and this finding has not been refuted). It’s long been known that cholesterol lowering is linked to diabetes. This article discusses the problems with the claims that high cholesterol is linked to breast cancer.
Unfortunately, doctors don’t get to hear about opposing viewpoints like those I’ve collected over the years. And they assume that the sheer weight of science behind the cholesterol theory must mean some of it is valid.
The trouble is, they know very little about how the science sausage is made.
Doctors Writing LDL Cholesterol Guidelines Need Money for Research
To elevate yourself to the status of guideline writer, you need to have a track record of published research. To do research, you need money. A lot of money. Where does the money come from?
For less than 3 seconds during Dr. Wong’s presentation, a slide flashed this disclosure: “Dr. Wong receives research support through his institution from Novartis, Regeneron, Novo Nordisk, and Lilly and is a consultant for Novartis, Agepha, Ionis, and Kaneka—all drug companies that make and sell cholesterol-lowering drugs or devices. These are just his currently active relationships, mind you.
This is not exceptional. Most of the experts who write guidelines and educate doctors take large sums of money from drug companies for their research.
Ordinary doctors, like myself, often assume research money comes from a neutral party, like the government or a University. That used to be the case. It used to be that scientists would frown on those who accepted money from industry. Having a financial relationship with companies selling cholesterol-lowering drugs when you are researching the benefits or harms of lowering cholesterol is called a conflict of interest for a reason. Most people are loath to bite the hand that feeds them.
Independent Physicians Call for Less Aggressive Cholesterol-Lowering Guidelines
Doctors who do not have ties to the industry periodically review the evidence and publish their findings. They generally conclude that aggressive cholesterol lowering with drugs is unfounded.
One such doctor is Dr John Abramson, from the Department of Health Care Policy at Harvard Medical School and a Robert Wood Johnson Public Health Policy Fellow. He first reviewed the evidence in 2013. He found no support for the use of cholesterol-lowering drugs in people with a less than 20 percent risk of a heart attack over the next 10 years.
Given the fact that statins have numerous side effects, taking a drug that won’t help you exposes you to risk without the possibility of benefit. A bad idea. It also violates the doctor’s dictum premium non nicer, first do not harm. Despite this controversy, conflict, and lack of evidence, guidelines today recommend that doctors consider cholesterol-lowering statins for people at much lower risk, 7.5 %
Well-funded Experts Slam Independent Reviewers
The British Medical Journal published the article in 2014 and it was immediately attacked. A Doctor named Rory Collins said that Dr. Abramson’s article may cause “very large numbers of unnecessary deaths from heart attacks and strokes.’” He further called for the government to step in and ensure the journal “to ensure the public gets accurate information on the risks and benefits of the potentially life-saving drugs.”
Merck had already paid Dr. Rory Collins over 200 million for research he’d done by that point in time.
Merck’s Zocor was the first ever blockbuster statin, released in 1992. More recently, they’ve invested billions in developing another kind of cholesterol-lowering drug called a PCSK-9 inhibitor. The only way to push LDL under 70 is to take multiple types of cholesterol-lowering drugs—for example, both a statin and a PCSK-9 inhibitor.
Doctors Unaware or Unconcerned About Conflicts of Interest in Science
Most doctors don’t read articles like Dr. Abramson’s; if they do, they don’t know what to make of them. Most doctors get their information from conferences and colleagues who have gone to conferences where they learn about the latest guidelines.
Dr. Abramson has not been invited to these sorts of conferences, nor has he been invited to craft any preventative medicine guidelines, despite having the perfect background. His research is rarely presented at these sorts of conferences.
Dr Rory Collins is a frequent flyer. Even when he doesn’t go, someone else will likely cite one of his 2,000-plus publications. His publications make their way into guidelines. The guidelines are not just guidance. Many doctors are financially penalized for nonadherence. I wrote about this years ago in an article on pay-for-performance programs.
Most doctors assume that the guidelines they follow are supported by evidence. I know this because I work with them and I see how many prescriptions they write for people at low risk of heart disease. I hear them in the other room saying to their patients with side effects that they need to take their prescriptions or they might die.
Conflicted Journal Editors Don’t Print the Whole Truth
Most doctors believe these conflicts of interest don’t matter because most doctors assume that the peer review process still works the way it used to. According to Dr. John Abramson’s book, Sickening, that’s simply not true. Journal editors need money from the pharmaceutical industry, too. So they are conflicted. This conflict means they don’t review the data they need to review anymore.
Unlike the authors of their articles who (sometimes) disclose their conflicts, the journals themselves do not. When subpoenaed during a lawsuit these entanglements might be exposed. This is how John Abramson discovered the truth that he reveals in his book.
What Can You Do?
It’s grown harder and harder to navigate the healthcare industry. Just getting an appointment with a doctor who accepts your insurance is a battle in itself. But it’s never been more important to be your own health advocate. Take the time to understand the role of cholesterol in the human body and the harms of statin drugs. The reality is you have a great deal of control over your health. Most of the bad diseases out there don’t come from family history or bad luck, as we usually assume. They come from our diet.
I’ve had to do a lot of work myself to understand this problem. Some of that has involved sorting out what causes heart attacks myself. And some of that has involved learning from other doctors.
There are now many doctors trying to warn the public that cholesterol does not cause heart disease. And others trying to warn the public that statins are not safe, nor are they effective. I’ve put together a library of some of the best for you here.
If you want to what to eat to take control of your health, I’ve written out 10 basic rules. If ten sounds like too much, don’t worry! The first two are the most important. Those two alone will get you 80 percent of the way there. The work you put into a few hours of learning will reward you a thousandfold!
This Post Has 11 Comments
Note: Please do not share personal information with a medical question in our comment section. Comments containing this content will be deleted due to HIPAA regulations.















Dr. Cate,
Your latest book is terrific. I just finished it and am restarting for read two.
Even though I’m a 71 year old seriously professional CFP (Certified Financial Planner), I also became a pretty active health coach back in 2015, cause I suddenly got T2D. That put me heavily online (in the deer stand back behind our house,…we live on a ranch) and led me to actually meet Jason Fung and exchange emails and phone call with him back then. I totally fixed my T2D in six months and that essentially turned me into a health coach. I’ve fortunately personally met many of you super-serious health care geniuses at conferences I’ve been to. Chris Knobbe and I have become dear friends. And Chris in on my prayer team these days for my S4 melanoma that’s in my left brain and left lung (only,…zero on skin). My initial brain surgery and left brain tumor renewal was 11.30.21. Incredibly, I’m still here, three years later, and still running my almost 40 year old financial planning practice in downtown Fort Worth, where I still do health coaching. I also give out many excellent healthcare books,…lately including Dr. Ovadia’s and Dr. Knobbe’s books, and most recently, your excellent new book.
I HAVE A MAJOR QUESTION FOR YOU. I’ve kinda regularly pushed back on my primary doc, for quite a while, on taking statins. Having said that, she recently had me do a bunch of artery testing that revealed I’m seriously, more than half stopped up on at least one heart artery, LM+LAD. She believes I really need to start Rapatha now (which I just did) to control that. Is she right?
She’s not a dummy, and she reads alot of books I do. I’m fixing to send her your latest one.
My nutrition these days is pretty heavily Dr. Seyfried based. I basically eat animal foods, mostly beef, fish, butter, tallow, cheese, cream, yogurt, and occational cottage cheese.
Unbelievably, my originally surgically removed left brain tumor is still gone, and on my left lung tumors, the smallest of the three is gone, and the larger and medium one are both half original sizes. We’re presuming the year of yervoy/opdivo worked on that, and I’m considered to be on remission. Yay.
My major current cancer related issue is that my left brain got seriously radiation hammered with five hardcore radiations right around where the 2″ diameter tumor, twixt left eye and left ear, had been removed. My second brain surgery on June 30 of last year, discovered those five fried brain spots and he actually scalpel removed four of them. The one remaining has two brain blood vessels going through it, so he avoided scalpeling that one. A brilliant neurosurgeon gal at UTSW/Dallas has me, for last six months, on daily vitamin E and Boswellia capsules to attempt radiation suppression. Based on my most recent left brain quarterly MRI, the radiation spread up there seems to be seriously slowing down. Yay!!!!
I’m so fortunate to be alive, and to have literally only missed two months of work after each of my two brain surgeries since this started three years ago.
My brain damage from the removed brain tumor is both anomic and receptive aphasias. That’s a rigorous issue to constantly deal with. As world traveling/speaking past president of the U.S.’s Financial Planning Association, back in 2001, I’ve got probably over 2,000 human names in my brain. I’ve got my ability to access them now back up to maybe 100 (from 10 family only names when this started in late 2021) people. I constantly have to look up my clients’ names,…even people I know well and have for decades. But, they love me and they understand!
Thanks for all your tremendous work, and for your help/thoughts on the Rapatha deal for me. Do I likely really need it?
Good for you for taking control of your health and not giving in to the statin fever. I can’t give you personal advice but I can tell you that cholesterol is not the cause of heart attacks or anything bad at all. They call it “bad” cholesterol, and that’s all they have to do to scare us. But it’s not bad. Here’s an article I wrote that I recommend you read! https://drcate.com/cholesterol-what-the-american-heart-association-is-hiding-from-you-part-1/
So much is being said in the last few years from the likes of Thomas Dayspring, and Peter Attia regarding the role of apoB.
What are your thoughts on this? (apoB and not the Drs…).
My experience has been that apoB correlates pretty clearly with my LDL, but these guys imply that getting apoB below 50 is essential, and mendelian randomisation shows clear casual links between cardiovascular disease and high apoB (they say).
Is this just more blinding by science, or is it new information that wasn’t clear in previous years?
What is Apo B? I describe it in this video here.
Sadly, most folks either don’t understand that basic concept of human metabolism or their thought processes are twisted and impaired by the unscientific narrative that cholesterol is “bad.”
Does HDL in the high hundreds impact health. In a news article there was a link of high hdl correlated to dementia.
I hadn’t seen that please share the article!
On p. 151 of Deep Nutrition, you talk about interpreting a standard lipid panel. Can you share how you came to these numbers?
HDL = 45+ men 50+ women
LDL = less than HDL x 3
triglyceride less than 150
Thanks!
HDL numbers are on the idea that high HDL reflects a healthy lipid cycle and an abundance published data showing that below 45 for men and 50 for women correlates with disease.
Triglycerides, same idea but opposite directions. High triglyceries reflect an unhealthy lipid cycle and published data.
LDL less than HDL x3 was based on the lipid cycle concept and my own clinical observations with thousands of patients. Yes I believe doctors can think for ourselves, we don’t always need data.
Great info, thanks. I’ve done a fair bit of reading on this topic. For anyone interested you can’t go past all the books by Malcolm Kendrick. The whole system is pretty disgraceful.
Thank you Dr. Cate. I will reference this post in the future.
My journey from the SAD way of eating to meat-heavy Keto looks like this:
SAD: TC 189, LDL 108, HDL 67, TG 53
Keto: TC 371, LDL 263, HDL 94, TG 43
Recent meat-heavy Keto: TC 597, LDL >450, HDL 95, TG 78, fasting glu 96,
A1c 4.9, Fast .Insulin. 4.3 (No statin, no Rx)
My wife has had many successes: losing almost 60 lbs, off BP med, stopped statin.
Dr. Cate’s “Fat Burn Fix” was the start of our journey and I am ever grateful!
Being 76, in a Medicare Advantage program, I have two mandated exams each year. This always involves lab work. My cholesterol is always high, with LDL hovering just below 200. However my triglyceride to HDL ratio is always under 2, typically around 1.6. The follow up from every exam is the same. My doctor is still recommending the horrifying DASH diet, even as she freely admits that I know more about nutrition than she does. Many of my neighbors are around my age, and most are diabetic or pre-diabetic, veering toward Parkinson’s and Alzheimer’s. I feel great, have no prescriptions, and start every day with 100 or more push-ups and a 5k walk. For this I thank Dr. Cate, Mark Sisson, Drs. Lustig, Gundry, and Johnson. Hat tip as well to Maria Cross, my nutritionist on Substack.