Infant formula is 98% ultra-processed oil, sugar, and protein powder. Homemade infant formula can help a child thrive in many of the same ways as breast fed babies.

Why does my stomach hurt? It could be functional constipation
Table of Contents
- Does an aching belly and constipation get in the way of your life?
- It’s called “chronic functional constipation.”
- What causes functional constipation?
- The Colon Can Start To Enlarge
- How to diagnose functional constipation
- How to treat functional constipation, with or without dilation
- Retraining Your Colon
- Shrinking A Dilated Colon
Does an aching belly and constipation get in the way of your life?
Do you get bloating and cramping feelings throughout the day?
Do you worry you might have a food allergy causing your stomach problems?
Today’s article was inspired by the story of a recent patient. A busy professional woman in her mid-forties who had been suffering from progressively increasing daily digestive discomfort for over fifteen years. She had been through food allergy testing and tried restricting the foods she was most sensitive to. She’d tried all kinds of diets. She’d tried probiotics. She’d tried herbal tea and fiber and laxatives. But nothing helped.
This article is continued below...(scroll down)
After listening to her full story and doing a complete exam, I told this long-suffering woman that I suspected she was suffering from THE MOST common cause of all tummy pain and belly aches that I see.
It’s NOT food allergies. It’s NOT gluten intolerance. It’s not even irritable bowel. What IS the number one most common reason for stomach aches and digestive problems?
It’s called “chronic functional constipation.”
Chronic means it’s been going on for a long, long time.
Occasional constipation is more familiar to most folks, and they usually know what exactly brought it on. Maybe you were traveling and couldn’t find a bathroom. Maybe you got dehydrated. Maybe you ate something that constipated you. This kind of ordinary constipation is called “occasional constipation” and is, by definition, brief and resolves in a few days.
When constipation doesn’t go away after you’re back into normal routines or after using of evacuation aids (like laxatives or enemas), and once it progresses to the point it becomes a chronic, long-term ongoing issue, then we call it “chronic functional constipation.”
Functional constipation may sound like a silly name. After all, how can constipation be functional? It’s called functional constipation to distinguish it from structural constipation caused by certain kinds of birth defects and other rare disorders. Functional constipation is very common in pediatric practice and is widely recognized as the number one cause of constipation in kids.
In adults, however, functional constipation often goes undiagnosed, sometimes for decades. Whether you’re two or 42, functional constipation has the same cause–and the same solution. To understand why treating functional constipation is more difficult than treating occasional constipation, we need to understand what causes functional constipation.
What causes functional constipation?
Constipation is a problem of the colon, which represents the last five feet or so of the entire roughly 30-foot digestive system. The small intestine breaks down your food so you can absorb the nutrients. This process uses enzymes and water–lots of water, over 2 gallons per day. This way, the small intestine is able to absorb most of the nutrition from your diet including protein, fats, vitamins, antioxidants, and salts. The colon re-absorbs most of that water and some of the remaining minerals. It houses the vast majority of the good bacteria in the gut. And serves as a poop storage facility until you find a convenient time to head to the bathroom and heed nature’s call.
And therein lies the problem. The colon is very patient. In some of us, it’s overly patient. Those with overly patient colons are prone to developing constipation.
You know that special urge you get when your colon is talking to you about finding a bathroom, soon? Well, how many times have you been too busy to head to the bathroom when you’re feeling that calling? When the feeling is uncomfortably strong, its called fecal urgency. There seems to be no name for just regular signaling, so I just call it the special urge.
You know what happens if you don’t go in response to the special urge, right? You miss your chance. If you’re having a really busy day, well the colon just buckles down, dilates a bit to hold more of the poop that your body is constantly creating, and waits until you decide the time is right.
If the time doesn’t come for a certain amount of time, well the overly patient colon just figures it won’t happen today and waits till the next day to send the signal again. If you are too busy the next day, it can wait some more. If you keep putting it off, it just keeps waiting. Eventually, in some of us, it will stop creating that special feeling altogether. And that’s when we can really get into trouble.
Kramer Has to Poop
One of Seinfeld’s writers must have suffered from functional constipation because he worked it into a skit that I find very helpful in understanding the importance of keeping up-to-date with the requests from your colon to spend some quiet time alone. Here it is:
Kramer missed his chance and now he can’t go. Normally ignoring the special urge just once, does not cause a problem. So my medical experience tells me that Kramer must have been ignoring his special urge for years and this set him over the edge.
The Colon Can Start To Enlarge
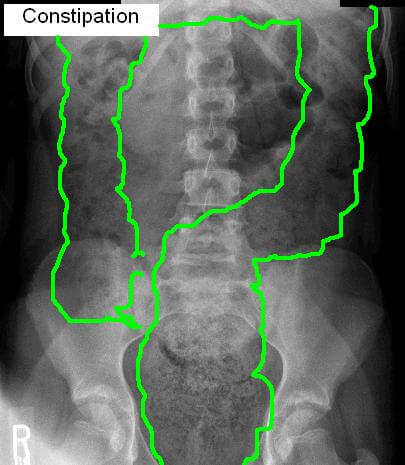
Missing the urge over and over again can have a disturbing consequence. Over time, like years, in a person with an overly patient colon, the colon will have to go beyond just dilating (stretching out like a balloon) to accommodate the extra stool it’s been asked to hold, it can actually grow bigger so it can hold more stool all the time (see Xray image, below)
And therein lies the reason why this disorder often goes unrecognized. Because when your colon is dilated and distended, you can feel it. But when your colon has grown larger but is not also distended, you don’t actually feel constipated.
Instead, you suffer from frequent cramping–because the colon has to work much harder to move all that stool along when its overly wide and overloaded. You can develop a bloated feeling because your colon holds bacteria too, trillions of them. And the more stool, the more bacteria you’ll house in your gut as well. A lot more, like two, three or even ten times as many. And all those bacteria are producing that much more gas. You may not even be expelling that much gas that often, but because your colon is dilated, it’s holding more gas. And the gas can collect in air pockets and cause localized distention and discomfort from time to time.
How to diagnose functional constipation
This should go without saying, but I do need to say it: This is not legal advice. No one should diagnose their digestive issues as functional constipation without first getting a proper evaluation and examination by a qualified practitioner to rule out other causes.
When it comes to finding a healthcare provider who will consider the diagnosis of functional constipation as the cause, however, that’s where it can get tough. Pediatricians see this issue all the time. So if you’re under 18, go see a pediatrician. If you’re 18 or older, see a Family Medicine physician. Family docs usually see kids too, and while you may need to prompt your family doc to consider the diagnosis of functional constipation in adults, he or she has learned about this disorder and should know how to treat it. If you have an Internal Medicine doctor or another specialist (even GI), they may not be so familiar with functional constipation, and it may be helpful to show this article to your doctor.
Here’s what I look for when I suspect functional constipation.
Abdominal exam: Sometimes when people are thin you can feel a movable blob in the lower left quadrant of the abdomen at the location of a part of the colon called the sigmoid. Sometimes there is mild tenderness throughout the entire belly. Most often the exam is completely normal.
XRay findings: When people are overweight enough that it’s impossible to really feel what’s in the abdomen, I rely on XRay. I also will get an XRay if I feel a mobile mass, to verify the presence of extra poop. I often show my patients their XRay as a visual aid to help understand that treating functional constipation is going to require a very different protocol than treating regular, occasional constipation.
How to treat functional constipation, with or without dilation
The treatment of functional constipation requires more diligence, patience, and consistency than the treatment of occasional constipation. You’re not just going to have to empty out a lot of extra stool. You’re going to have to give your colon time to shrink up again to get back to its normal size. And you’re also going to have to maintain that normal-sized, smaller colon or you will just develop the same problem again.
To accomplish both, you’re going to have to retrain your colon to get back in the habit of sending you the special signal again. The best way to revive the special signal is to pick one mealtime per day that you can head into the bathroom for a few minutes of quiet, private time. Just like when you’re potty training a toddler–you don’t wait until he tells you he has to go number two. You just plunk him on the toilet with something to keep him entertained. This does more than teach your toddler cognitively; you’re also teaching the nervous system in his belly (called the enteric nervous system) that after breakfast (or whenever you have chosen) is the time it gets to do its thing.
Retraining Your Colon
The key is consistency. You don’t want to do breakfast one day, then lunch the next, then dinner. It has to be the same ritual trip to the bathroom after the same meal, over and over again, or the colon just won’t learn.
Retraining your colon once you’ve developed functional constipation will typically require two steps.
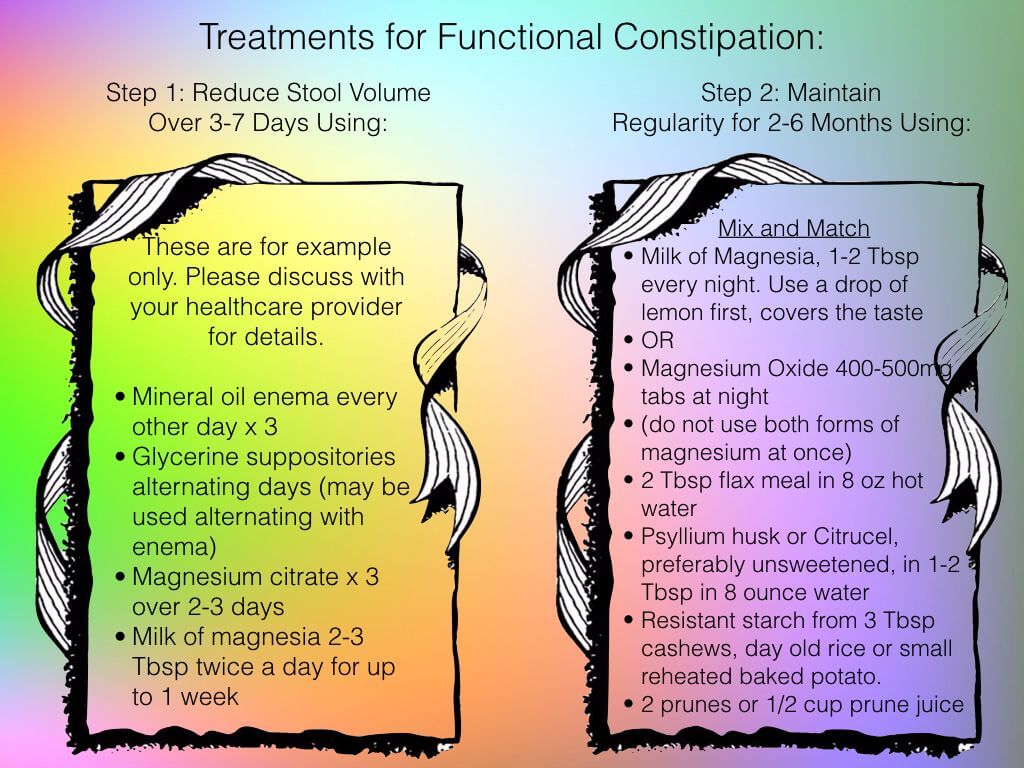
The goal of step one is to get to the point where your body’s stool volume is back to normal. This can take days or, in severe cases, even weeks. I’ve written out some of the therapeutics I use for this stage to give you an idea of how aggressive you need to be. NOTE: I do not use all of the bulleted items, usually just one or two.
After providing the Step One protocol, I usually see people in follow-up and do a repeat exam to determine if we have achieved the goal of reducing the body’s stool volume to normal or if we need to continue for another week or so with this more aggressive therapy.
Shrinking A Dilated Colon
Then we formulate a program for step two. The goal of step two is to allow the overgrown colon to shrink back to a normal size. During step two you will need to be able to evacuate every day. You will most likely need to take something every day to accomplish that. I’ve included what I find useful for this stage in the image above as well. NOTE: I do not use all of the bulleted items, usually just one or two.
The Poop Rock
Before you embark on any treatment, if this has been an issue for a long enough to dilate your colon, you may have developed another complication of chronic functional constipation called a fecalith. Fecalith is Latin for “fecal stone” and that hopefully gives you an idea of how hard it can be to break up and evacuate this resistant waste material. A fecalith is a hardened area of stool that may be too large to evacuate and requires a rather intensive protocol to break up, including enemas, suppositories, and aggressive oral laxatives.
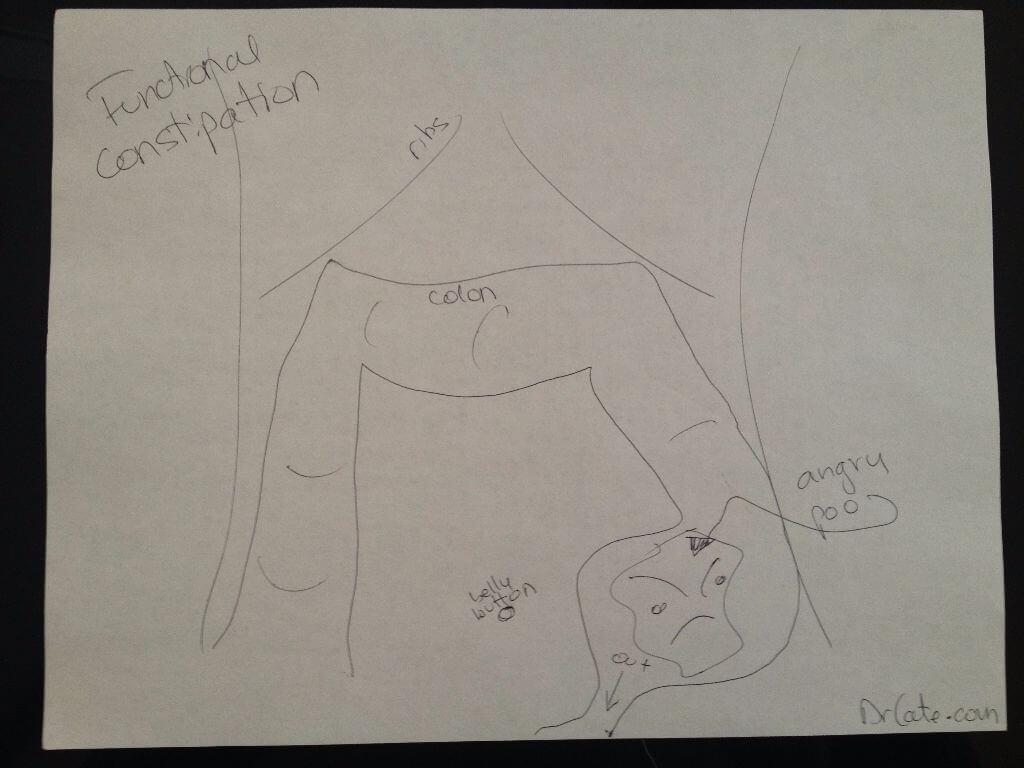
Showing a child an image of why their tummy hurts can help get them on board with the treatment. Even without a fecalith, the stool in the sigmoid can be very dry, hard, and difficult to pass, and behave like “angry poo.”
When I’m working with kids I usually like to explain a fecalith as “angry poo” and draw a cartoon of the relevant anatomy so they can get on board with the treatment plan because they need to be on board or you will have a tougher time clearing the problem.
I generally start with 3-4 enemas over 2-4 days, suppositories for the balance of a week and oral magnesium citrate solution for the full 7 days. Such intensive therapy can easily cause dangerous fluid or electrolyte imbalances in small children or anyone with kidney, heart, or liver disease. So I do not advise attempting to break up of fecalith without professional help.
The total treatment time for functional constipation usually requires 4-8 months and several visits. But you can expect a complete recovery. Just remember, your colon requires your cooperation to function at its best. If you give it just a little time every day to do its thing, you’ll have the rest of the day to do everything else you want!
Please note: Please do not share personal medical information in a comment on our posts. It will be deleted due to HIPAA regulations.
This Post Has 11 Comments
Note: Please do not share personal information with a medical question in our comment section. Comments containing this content will be deleted due to HIPAA regulations.
















What do you mean by mineral oil 3xs? Mineral oil 3xs daily? Can you substitute organic olive oil?
What do you mean by mineral oil every other day x 3? Thank you Stacey
I had a colon resection due to a prolapsed colon. I suffer horribly with gas that the pain is so bad I feel like it’s my gallbladder! The pain shots up to my rib cage. I have 2 hernias now a umbilical, and upper larger one that was already fixed with mesh but it came back out. I don’t have a bowel movement’s for 7 days sometimes. I need help bad but enemas don’t work. I don’t think the plan above would work for me. Any help?
Hi Dr. Cate,
I’ve been diagnosed with ulcerative colitis for the past 2 years, and have completely changed my diet and life style. I am a 25 year old male who enjoys dividing my time between training hard in the gym and playing basketball. Naturally, I have a very thin frame and have always been obsessed with trying to put on healthy muscle/weight.
What type of diet would you recommend that will still help me achieve the healthy muscle and weight I am looking for?
Thanks!
Jesse
Hi Dr. Cate,
I’ve been diagnosed with ulcerative colitis for the past 2 years, and have completely changed my diet and life style. I am a 25 year old male who enjoys dividing my time between training hard in the gym and playing basketball. Naturally, I have a very thin frame and have always been obsessed with trying to put on healthy muscle/weight.
What type of diet would you recommend that will still help me achieve the healthy muscle and weight I am looking for?
Thanks!
Jesse
What are your thoughts on Blackcurrant Seed Oil?
Why does the rice have to be a day old?
Not sure where you saw that, my post or another comment?
2nd to the last option of Step 2 column.
Dr. Cate…what if you already go once a day with no problem, but are still bloated and gassy, can still feel the lump (I’m only 100 lbs) and always feel way better after going a 2nd time when that occasionally happens? I’ve tried milk of magnesia, magnesium supplements, fiber supplements, and the supplement Calm, but they just make me more bloated. I eat a very healthy diet with lots of fruit and veggies, drink about 80 oz of water a day and exercise 4-5 days a week. Do you think 2 prunes a day will help me go twice a day?
Gosh sounds like you need a pelvic exam (if female) or other evaluation by your doctor. I hope you’ve gotten one by now if the problem has not resolved !!!